Osteomalacia or “soft bones” is a condition that affects your bones and is most often due to a lack of vitamin D and sometimes due to a mineral deficiency. When found in children, this condition is called rickets. Nowadays it is rare to see rickets, but osteomalacia is still a threat to adults.
Osteomalacia interferes with new bone formation or the production of osteoblasts (bone cells). The human body is constantly removing old bone and replacing it with new bone. This is called “bone remodeling” and osteomalacia interferes with this very important process. To perform bone remodeling, your bone needs…
- Minerals (calcium and phosphorus)
- Bone protein matrix (osteoid, made up of collagen)
Osteoid is the bone protein matrix and when there is insufficient mineral or osteoblast dysfunction, the collagen in the osteoid does not mineralize properly, and it accumulates. If bone is made up of more collagen than minerals, bones become soft and increased risk of fracture.
- Osteoclasts (bone removing cells)
- Osteoblasts (bone producing cells)
The Bone Remodeling Cycle
Your bones are dynamic tissues that are constantly undergoing the remodeling process. Old bone is resorbed by osteoclasts and new bone is laid down by osteoblasts. This necessary process acts to repair bone microdamage that occurs normally through daily activity. It also acts to replace bone during the growth process and following fractures.
This back and forth signaling between osteoblasts and osteoclasts is crucial for this process to work and be effective.
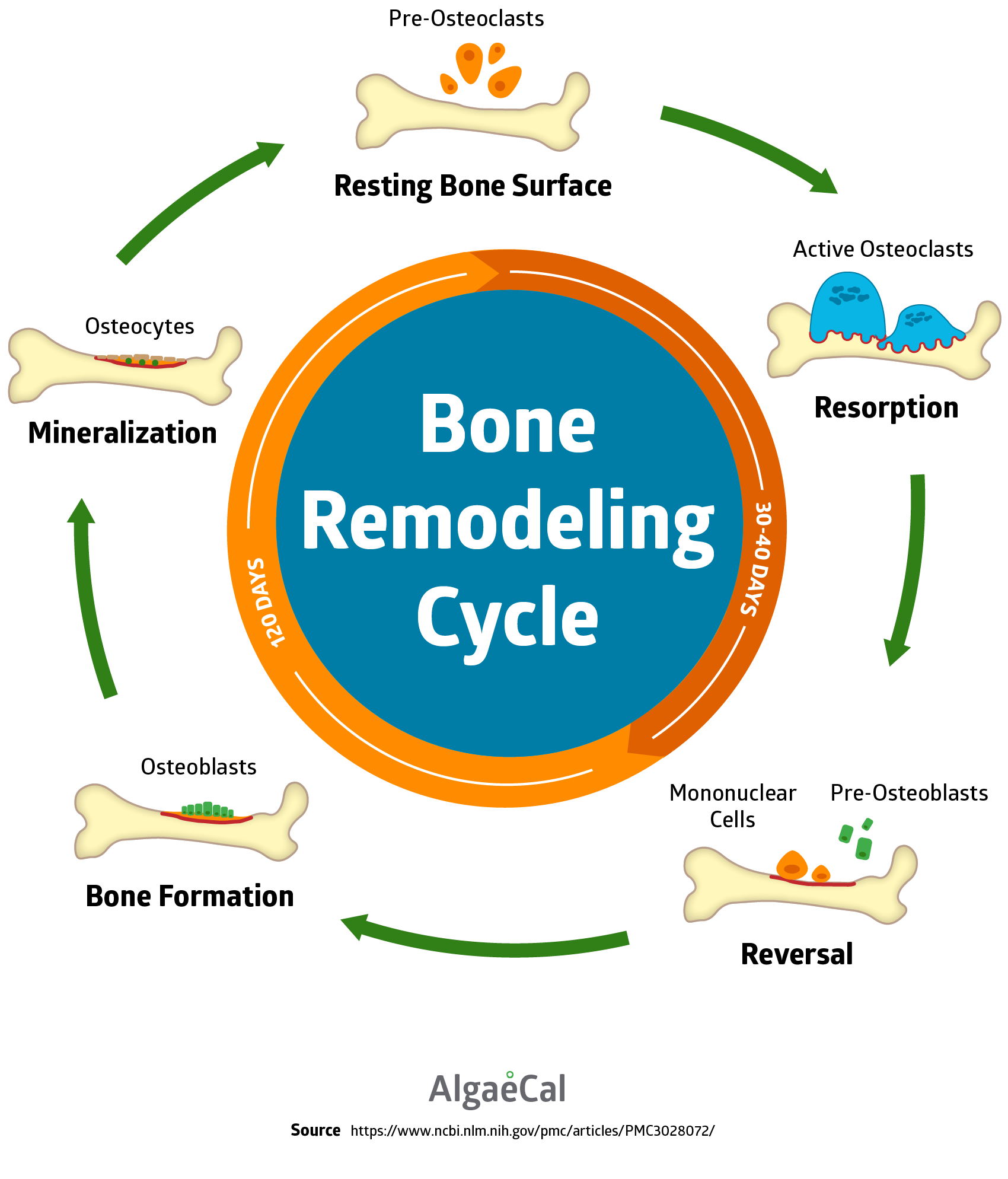
- Resting: The resting stage is when the bone surface is inactive and covered by bone lining cells.
- Activation: This stage exposes pre-osteoclasts to the mineralized bone surface. These pre-osteoclasts are recruited and taken to the resorption site.
- Resorption: When osteoclasts make contact with the bone surface they become active and begin the resorption stage of the cycle.
- Reversal: Once the resorption stage is complete, there is a period of about 1-2 weeks before formation begins and is called reversal.
- Formation: This stage happens in two stages. First is the synthesis of bone matrix by osteoblasts. Second, is the subsequent mineralization of the matrix.
* If there is an imbalance between the resorption and formation stage, it can lead to bone loss and diseases such as osteoporosis and osteomalacia.
What Are The Causes and Risk Factors of Osteomalacia?
Bone mineralization requires adequate minerals (calcium, phosphorus and vitamin D). Inadequate amounts of any one of these will develop into osteomalacia. Here is a list of the known causes of osteomalacia.
Lack Of Vitamin D In Diet
Vitamin D3 is a difficult vitamin to get adequate amounts from diet alone. For instance, a 3-ounce sockeye salmon filet only contains about 450 IU of vitamin D3. Some mushrooms, like Portobello, will give you 400 IU of vitamin D3 per 3-ounce portion. Not entirely insignificant, but not enough.
You may not get enough vitamin D from your diet if you:
- Are lactose intolerant or are sensitive to dairy (where you have trouble digesting milk products)
- Do not eat or drink milk products (more common in older adults)
- Follow a vegetarian diet (Fish, organ meats, and eggs are high on the list of vitamin D food sources)
- Are not able to absorb vitamin D well in the intestines, such as after gastric bypass surgery.
Lack Of Exposure To Sunlight
The latitude of where you live plays a role in the amount of vitamin D-producing UVB light that reaches the earth’s surface. This is crucial during the winter months or seasons when the sun isn’t as readily available because of the low angle of the sun. In Boston for example, little if any vitamin D is produced by the skin during the months of November through February. Take into consideration shorter days and clothes covering skin, which also limits the UVB exposure.
That doesn’t mean if you are living in lower latitudes that you’re off the hook. Individuals living in relatively sunny environments are still at risk for vitamin D insufficiency. Studies in South Florida, South Arizona, and Hawaii found significant levels of the population had low vitamin D levels, despite abundant sun exposure.
Factors that can undermine vitamin D production include:
- Desk jobs: Where one is working indoors during daylight hours.
- Skin color: Those with darker skin are more likely to have lower levels of vitamin D.
- Use of sunscreen – in theory: Sunscreen is used to block the UVB light and prevent sunburn. However, an often-cited Australian study showed that during an Australian summer, there was no difference in the vitamin D levels of adults who were randomly assigned sunscreen compared to those who were assigned the placebo cream.
- Vitamin D Absorption Problems – The health of your gut can influence the amount of vitamin D you can absorb. If you suffer from Celiac disease, Crohn’s disease, cystic fibrosis and chronic pancreatitis your vitamin D absorption may be reduced. In addition to your gut and digestion playing a role in vitamin D absorption. The following are also factors that influence vitamin D status:
Liver and Kidney Health
Some types of liver disease can reduce vitamin D absorption while other types block essential steps for vitamin D metabolism to occur.
Certain Drugs
Common drugs used to treat seizures such as phenytoin and phenobarbital and cholestyramine and colestipol for hypercholesterolemia inhibit vitamin D absorption.
Specific Surgeries
Gastric bypass surgery not only reduces the size of your stomach but also your ability to absorb nutrients. Furthermore, it eliminates your ability to absorb fat-soluble vitamins D and K.
Phosphate Deficiency
A diet lacking phosphates can cause phosphate depletion and lead to osteomalacia. Foods high in phosphorous are pumpkin seeds, brazil nuts, romano cheese, and salmon. Blood tests can be done to test your vitamin D and phosphate levels.
Risk Factors For Osteomalacia
- Hereditary vitamin D metabolism disorders
- Kidney failure
- Mineral deficiency
- Cancer
- Liver disease
What are the Symptoms of Osteomalacia?
At the very early stages of osteomalacia, there may not be any symptoms at all. But once it progresses, osteomalacia can cause individuals to waddle (with a side-to-side stride). In addition, one may experience…
- Fractured bones due to minimal trauma
- Lethargy
- Stiffness
- Muscle Weakness: Muscle weakness tends to affect the thighs and the muscles in the shoulders and main core of the body.
- Difficulty walking up stairs or getting up from a seated position.
- Bone Pain: Such as dull aches, especially in your hips. Pain is most often felt in the legs, groin, upper thighs, knees and sometimes in the feet. In some cases, the pain will be the result of partial fractures, which are only visible on x-rays.
If you have low blood calcium levels, you may also experience:
- Hand and foot spasms
- Irregular heart rhythms
- Numbness in your legs and arms
- Numbness around your mouth
However, the symptoms can often be confused with other conditions and lead to osteomalacia being misdiagnosed frequently.
How is Osteomalacia Diagnosed?
See how these symptoms could also be for other conditions? It makes it tricky. So to be sure, it’s important to get tested.
Osteomalacia can be diagnosed by:
- X-Ray – Slight cracks in your bones that are visible on X-rays are characteristic of osteomalacia.
- Blood Tests – These tests will measure low levels of calcium, phosphorus, electrolytes and vitamin D in your system. A blood test can also be measured for Alkaline phosphatase isoenzymes and parathyroid hormone levels. High levels of these indicate osteomalacia.
- Bone Biopsy. This is a test where a small sample of your bone is removed. Although accurate, it’s rarely needed to make the diagnosis for osteomalacia.

What Are the Available Treatments for Osteomalacia?
Osteomalacia is often caused by a lack of vitamin D and sometimes mineral deficiencies. To treat osteomalacia, naturally, you need to:
- Get sufficient sunlight: You can boost your vitamin D by spending more time in the sun. Although be sure to discuss this with your doctor. Too much sun can increase your risk of skin cancer.
- Eat Vitamin D Rich Foods: Cold water fatty fish like salmon, sardines and tuna, eggs, liver and fortified foods like cereal, milk, and yogurt are some of the top food sources of vitamin D.
- Treat the cause: If your body has a difficult time absorbing vitamin D and other nutrients, you need to discover the root cause and hopefully, treat it. Most likely, you’ll need to take larger doses of calcium and vitamin D.
- Supplement: Changes in diet and lifestyle will positively affect your bones, but make sure to supplement for any shortfall they may have. AlgaeCal Plus is clinically supported to increase bone density in as little as 6 months – at any age! It contains ALL 13 known essential bone supporting minerals, including calcium from a plant source. And AlgaeCal Plus also provides vitamins C, D3, and K2. Osteomalacia is often caused by lack of vitamin D, but can also be due to other mineral deficiencies. Protect yourself and your bones starting today.






Mary Jo VanDeventer
March 12, 2019 , 1:17 pmThis article is informative. Thank you.