You know that omega 3s help protect your heart and your mind, right? So that’s not what we’re discussing today…
No, today I want to talk to you about a lesser-known role of omega 3s. How they help prevent your body from producing fat instead of muscle and bone as you age!
Sounds great, right? But there’s a small catch you need to know about to make the most of this benefit. You need to make sure you’re balancing your omega intake properly.
Let me show you how it all works…
Why Your Bones and Muscles Turn to Fat As You Age
To understand how omega 3s prevent sarcopenia (the medical term for when muscle is increasingly replaced by fat), you have to be familiar with a few key players.
In our article on omega 3 fatty acids and osteoporosis, we introduced omega 6s, the counterpart to omega 3s.
Now, omega 6s promote inflammation, while the omega 3s lessen it. Think of these two fatty acids like yin and yang. When they’re in balance, your body is at peace. Specifically, pro-inflammatory and anti-inflammatory signals are balanced. (More on this a little later on!)
The other key player is your mesenchymal stem cells (MSCs). MSCs are bone marrow cells that can grow up to be either osteoblasts (bone-building cells) or adipocytes (fat cells).
Here’s the thing: MSCs are easily influenced.
If they interact with anti-inflammatory omega 3s, they’re likely to become osteoblasts. But if they meet omega 6s, they tend to grow up to become adipocytes!
What’s more, researchers have discovered that MSCs are sensitive to aging.
In young to middle-aged individuals, MSCs saw moderate inflammation as a sign to build less fat and more bone. But in older adults, this situation reversed! MCSs exposed to inflammation built more fat instead of bone.
In addition, MSCs capacity to grow up at all — whether into an osteoblast or adipocyte — decreases as you age. Plus, the MSCs that do manage to grow up tend to choose the easier life of the fat cell.
All of these factors add up and contribute to the body’s tendency to produce less bone and more fat as you age. That sounds pretty bleak, doesn’t it?
But here’s the good news:
You can prevent this from happening by enlisting the help of the omega 3 fatty acids! When you consume enough omega 3s to balance your intake of omega 6s, you greatly lessen your risk of sarcopenia.
Read on for an explanation of how this works and to discover the ideal balance of omega 3s to omega 6s!
How a Balanced Intake of Omega 3s and Omega 6s Prevents Sarcopenia
It’s all about healthy competition.
Omega 3s parent compound, alpha linolenic acid (ALA), and omega 6s parent compound, linolenic acid (LA), partner with the same enzymes to produce their offspring.
So when omega 3s and omega 6s are around in balanced amounts, they compete for these enzymes! When the omega 3s win, they’re used to produce powerful anti-inflammatory offspring. And when the omega 6s win, they’re used to make pro-inflammatory offspring.
That’s why a balance of omega 3s and omega 6s means a balance of both anti-inflammatory and pro-inflammatory offspring.
To be more specific, omega 3s protect you from inflammation in two ways:
- The omega 3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), help prevent inflammation by competing for the same enzymes that would otherwise be used to produce pro-inflammatory compounds from omega 6s.
- EPA and DHA use these enzymes to produce their own anti-inflammatory children: the resolvins and protectins. These children are aptly named! Resolvins resolve (shut down) the inflammatory process. And protectins protect you from the harmful effects of chronic inflammation.
So how does this prevent sarcopenia?
Well, if you recall, MSCs are influenced by their environment. When they’re exposed to an anti-inflammatory environment, they’re more likely to become bone-building cells instead of fat cells. And a balance of omega 3s and omega 6s promotes an anti-inflammatory environment!
Remember, this balance is especially important for older adults because MSCs lean towards becoming fat cells as you get older.
To sum things up, a balanced intake of omega 3s to omega 6s helps protect you from obesity, sarcopenia, and bone loss. We’ll go over what the right balance is in a moment…
But first, let’s take a closer look at how this whole process works!
The Events that Lead to Inflammation and Sarcopenia or Healthy Bone and Muscle Mass
Don’t be intimidated by how complex the following diagram looks! We’re going to break it down step by step.
But to give you a broad overview, this diagram looks at:
On the Left Hand Side
- The parent compound of the omega 6s, linoleic acid (LA).
- LA’s pro-inflammatory child, arachidonic acid (AA).
- AA’s pro-inflammatory offspring: prostaglandin E2 (PGE2) and leukotriene B4 (LTB4).
- How AA is modified by COX-2 or 5-LOX to produce their pro-inflammatory offspring.
On the Right Hand Side
- The parent compound of the omega 3s, alpha linoleic acid (ALA).
- ALA’s anti-inflammatory children, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
- EPA’s anti-inflammatory offspring: prostaglandin E3 (PGE3) and leukotriene B5 (LTB5).
- How EPA and DHA are modified by COX-2 or 5-LOX to produce their anti-inflammatory offspring.
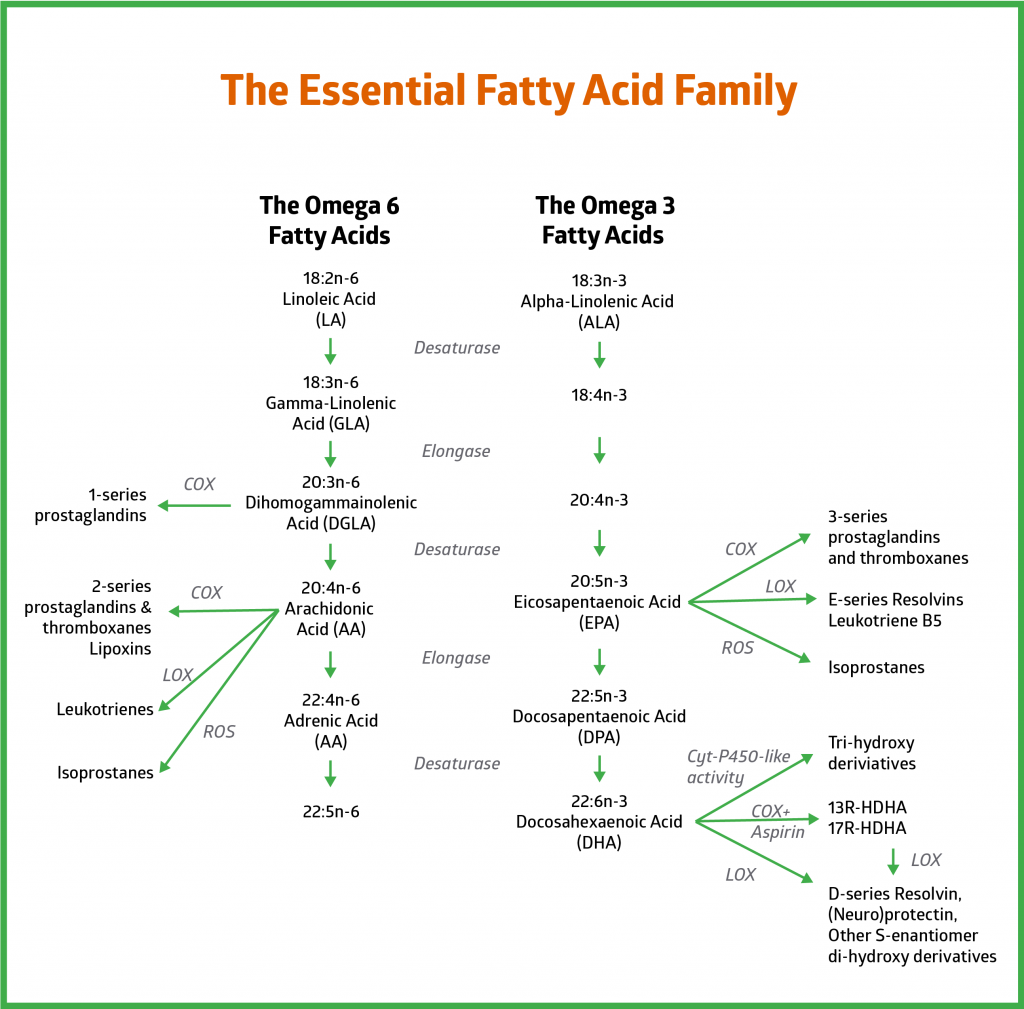

Linoleic Acid (LA) and the Omega 6s
Let’s start with the left hand side of the diagram.
You’ll see linoleic acid (LA) at the very top of the left column. This is the parent compound of all the omega 6s.
Three steps down from LA, you’ll find arachidonic acid (AA), the key pro-inflammatory child of the omega 6s.
AA partners with enzymes to produce two potent pro-inflammatory offspring: prostaglandin E2 (PGE2) and leukotriene B4 (LTB4).
- PGE2 is produced from AA by an enzyme called cyclooxygenase-2 (COX-2). Specifically, by a special form of this enzyme called “inducible COX-2” because it’s production is induced by inflammation. Simply put, your body make this version of COX-2 in response to inflammation.
- LTB4 is produced from AA by a different enzyme called 5-lipoxygenase (5-LOX).
These grandchildren of LA (the parent omega 6) really get the inflammatory troops rolling. In fact, both PGE2 and LTB4 are strongly associated with postmenopausal bone loss and obesity.

Alpha Linoleic Acid (ALA) and the Omega 3s
Now, let’s look at the right hand side of the diagram. (You’ll see it mirrors the left hand side in many ways!)
At the very top of the right column, you’ll see alpha linoleic acid (ALA). ALA is the parent compound of all the omega 3s.
Three steps down from ALA, you’ll find eicosapentaenoic acid (EPA), the first anti-inflammatory child of ALA.
EPA partners with enzymes to create two highly anti-inflammatory children: prostaglandin E3 (PGE3) and leukotriene B5 (LTB5).
- PGE3 is produced from EPA by the same enzyme used by the omega 6s, COX-2.
- LTB5 is also produced from EPA by the same enzyme used by the omega 6s, 5-LOX.
The key point here is that the same enzymes, COX-2 and 5-LOX, are used to produce both the pro-inflammatory offspring of AA and the anti-inflammatory offspring of EPA.
Also note the last omega 3 in the column, docosahexaenoic acid (DHA). DHA produces the anti-inflammatory resolvins and protectins, with the help of COX-2 and 5-LOX.
So, by understanding what turns these enzymes on, we can figure out how to point them in the right direction! Simply put, we can encourage them to work with anti-inflammatory EPA and DHA instead of pro-inflammatory AA.
The COX-2 Enzyme
COX-2 has a split personality, like Dr. Jekyll and Mr. Hyde.
COX-2 activity can either protect or damage your bones. It all depends on what triggers this enzyme!
If COX-2 encounters pro-inflammatory triggers, then Mr. Hyde comes out. That is, COX-2 gets up to no good and partners with AA to produce pro-inflammatory PGE2 offspring.
But if anti-inflammatory EPA is around, COX-2’s Dr. Jekyll side shows up. That is, COX-2 is on its best behavior and partners with EPA to produce anti-inflammatory PGE3 offspring. In fact, COX-2 in Dr. Jekyll mode is essential for the production of both of EPA’s anti-inflammatory children: PGE3 and LTB5.
What’s more, DHA needs COX-2 to produce its anti-inflammatory children: the resolvins and protectins.
COX-2 can even play an anti-inflammatory role with omega 6s! If you refer back to the left hand side of the diagram, you’ll see the first child of the parent omega 6 compound LA, is gamma linolenic acid (GLA). Now, GLA gets converted into dihomo gamma linolenic acid (DGLA).
Here’s where things get interesting: COX-2 as Dr. Jekyll can convert DGLA into the anti-inflammatory PGE1 series! But as Mr. Hyde, COX-2 converts DGLA into pro-inflammatory AA, which then generates the pro-inflammatory PGE2 series.
So COX-2 has the power to produce both anti-inflammatory and pro-inflammatory compounds from omega 6s. Plus, it can produce even more anti-inflammatory compounds from omega 3s.
But what brings out the Dr. Jekyll side of COX-2?
A healthy balance of omega 3s and omega 6s! Many experts believe the optimal ratio of omega 6s to omega 3s is 4:1. For more information on why this is the ideal ratio, visit our page on The Modern Omega 6 to Omega 3 Ratio and How to Fix It.
The main takeaway is that it’s all about balance:
- When there are sufficient omega 3s to balance omega 6s, COX-2 acts as both Dr. Jekyll and Mr. Hyde.
- As Dr. Jekyll, COX-2 produces anti-inflammatory offspring. These offspring resolve inflammation and encourage MSCs to become bone-building osteoblasts instead of fat cells. As Mr. Hyde, COX-2 produces pro-inflammatory offspring. These offspring ensure your immune system is active and ready to come to your defense.
- They also make sure your osteoclasts are put to work, but only long enough to clear out old or damaged bone and promote healthy bone remodeling.
- So when your omega 3s and 6s are in balance, so are the pro-inflammatory and anti-inflammatory actions of COX-2!
The 5-LOX Enzyme
Take another look at the diagram, and you’ll see the same story unfolding with the 5-LOX enzyme.
On the diagram’s left side, 5-LOX partners with AA to produce pro-inflammatory offspring called the leukotrienes.
On the diagram’s right side, 5-LOX works with EPA to produce the anti-inflammatory E-series resolvins and LBT5. It also partners up with DHA to produce the anti-inflammatory D-series resolvins and protectins.
As you can see, 5-LOX has a split personality just like COX-2. Depending what triggers this enzyme is exposed to, it can produce either pro-inflammatory or anti-inflammatory offspring. So once again, it’s all about balance.
When you have the right balance of omega 3s to omega 6s, 5-LOX’s anti-inflammatory and pro-inflammatory actions are also balanced.
Incidentally, this explains why the research on omega 3s and muscle mass is often misleading. More on this in the next section!

Why the Research on Omega 3s and Muscle Mass is Misleading
Many studies have looked into the effects of omega 3 supplementation on bone and muscle mass. And the results have been mixed. In fact, a recent meta-analysis found that omega 3 supplementation produces insignificant effects.
But this conclusion is flawed. Here’s why:
High levels of omega 6s may limit the effectiveness of omega 3s. Once again, it all comes back to balance!
You need a balanced ratio of omega 6s to omega 3s to see the benefits of these fatty acids. But if your levels of omega 6s are too high, basic supplementation with omega 3s won’t be enough to offset the pro-inflammatory environment. And many people in the Western world have high omega 6 levels. (We’ll touch on why in the next section.)
So it makes sense that the results of omega 3 supplementation studies would be mixed.
But there’s also growing evidence in favor of omega 3s supporting bone and muscle mass. A recent review looked at the effects of omega 3s on older adults in particular. Researchers concluded that omega 3s from fish oil improved muscle mass in older adults. And that omega 3 supplementation may also improve strength and muscle function.
Now, this is important because your skeletal and muscular systems are closely linked. Your bones are surrounded by muscle, and muscle contractions condition your bones. So stronger muscles equals stronger bones… and vice versa!
Omega 3s, Bone, and Muscle Mass Takeaways
Getting plenty of omega 3s is increasingly important as you age.
On top of fighting inflammation and promoting bone-building, a balanced intake of omega 3s helps prevent your muscles from turning to fat. In other words, it prevents sarcopenia— a major cause of bone loss and loss of independence in older adults.
Unfortunately, the modern Western diet (also called the standard American diet or SAD) promotes sarcopenia. That’s because the SAD is loaded with omega 6s, and is sorely lacking in omega 3s. For a more detailed explanation of why this is, visit our page on The Modern Omega 6 to Omega 3 Ratio and How to Fix It.
The main takeaway here is that a balanced ratio of 4:1 omega 6s to omega 3s:
- Lowers inflammation
- Prevents sarcopenia
- Encourages just the right amount of bone break down and bone-building to maintain healthy bones!
[ac_banner name=”fm-triplepower-2″]





Janet
June 10, 2019 , 5:36 pmSo I take this as we need to take an omega 3 supplement? I want to make sure I’m taking everything that I need to b